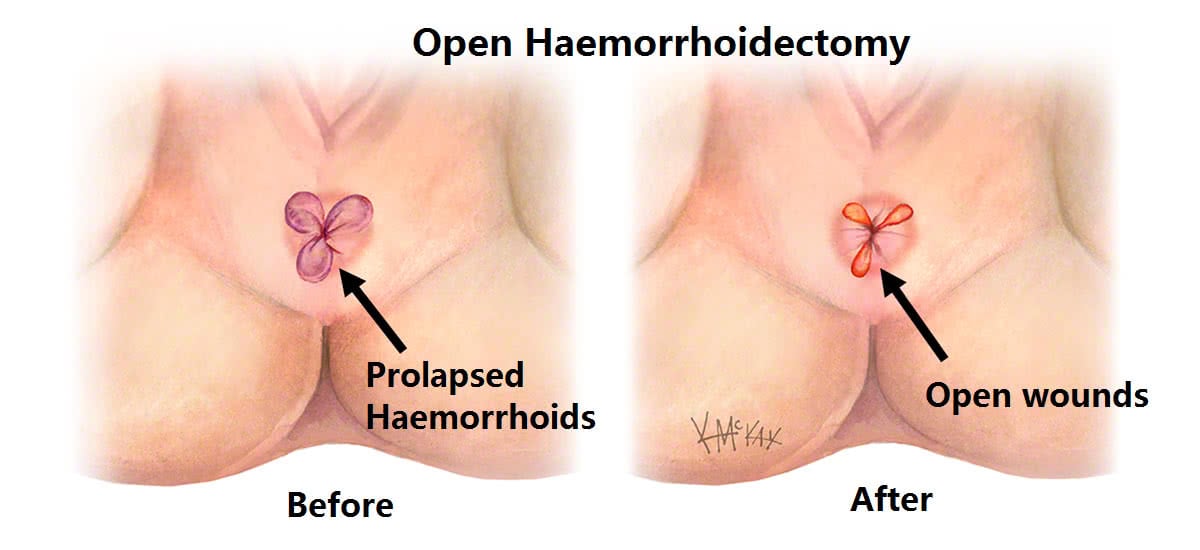
Haemorrhoidectomy involves the surgical removal of haemorrhoids. Traditional haemorrhoid surgery (Milligan Morgan Haemorrhoidectomy) is often quite painful as it involves cutting the haemorrhoids out leaving a number of open wounds. Stapled haemorrhoidectomy has the advantage of less pain and the avoidance of an open external wound.
Stapled haemorrhoidectomy
Stapled haemorrhoidectomy uses a circular stapling device that removes a ring of haemorrhoid tissue and mucosa (much like a doughnut) within the upper anal canal. This has the benefit of avoiding an open wound and having less pain than an open haemorrhoidectomy (when stapler positioning is high in the anal canal). It is only suitable for internal haemorrhoids of moderate size. It is not suitable for very large haemorrhoids, or those with significant prolapse or external component.

Traditional haemorrhoidectomy
Haemorrhoidectomy is the surgical removal of haemorrhoid tissue. As you look at the anus, most haemorrhoids are located in the 3, 7 and 11 O’clock position. Excision of these three haemorrhoid cushions leaves three raw sores that are said to give the appearance of a “clover” (Fig 2). Amazingly these sores, with the aid of warm to hot salt water (Sitz) baths, always heal, but can be painful in the first few days following surgery.
What to expect pre and post operatively for haemorrhoidectomy
Fasting and Bowel Preparation
Unless you are also having a colonoscopy, a normal diet without bowel preparation, is required the day before surgery. You need to fast from midnight the night before if your surgery is scheduled for the morning, or from 7am if scheduled for the afternoon. You will be admitted as a day-stay procedure. You will receive a fleet® enema 1 hour prior to your haemorrhoid operation.
Recovery and transport
Following your procedure, you will recover for an hour until the effects of sedatives have worn off. You should not drive yourself home after your procedure and should have someone organised (a friend or relative) to accompany you.
Bleeding
Spotting of blood will occur for 5 days following you procedure, and a sanitary napkin will be needed to prevent staining of your underwear. Bleeding will typically occur after opening your bowels. If the bleeding is more than a couple of teaspoons a day, notify your surgeon. Bleeding following rubber band ligation typically occurs 7-9 days following banding, and may require a course of 400mg of metranidazole (Flagyl®) three times a day for 5 days to settle it down.
Laxatives
You should remain on regular laxatives and simple analgesics for 1 week. A tablespoon of natural isphagula husk (Metamucil® or Fibogel®) twice daily, and 30ml of lactulose (Duphalac®) twice daily is recommended.
Pain control
For pain, a nonsteroidal is recommended such as 400mg of ibuprofen (Brufen®) along with 2 tablets of paracetamol. This should be taken regularly three times a day for five days. Opioid medications (Endone®) may sometimes be needed, but should be used sparingly as they cause constipation. Glycerine trinitate (Rectogesic®) ointment applied topically to the anus three times a day can be useful in preventing anal sphincter spasm.
Sitz Baths
Twice daily warm to hot salt water (Sitz) bathing to the anal region is soothing and antiseptic, and should be done for 1 week following your procedure. Put a handful of salt into a shallow bath of warm-to-hot water and sit there for 10-15 minutes.
Follow-up
You should follow up with your colorectal surgeon in 6-8 weeks following your surgery to review your wound and discuss further management if indicated.
