What is gastroscopy?
Gastroscopy involves the insertion of a fibre optic gastroscope through the mouth into the oesophagus, stomach and duodenum (first part of the small intestine). It is a non-invasive procedure that is safe and done under sedation.

When is gastroscopy indicated?
Gastroscopy may be indicated if you have a history of epigastric pain or bloating, or gastro-oesophageal reflux, or there is a family history of gastric or oesophageal cancer.
What is oesophagitis?
Oesophagitis may result from gastro-oesophageal reflux disease (GORD) where the acidic gastric contents reflux into the distal oesophagus. It is common in those with a hiatus hernia. The diagnosis is made during gastroscopy with red patches (erythema) or even ulceration of the mucosal lining of the oesophagus, with biopsies confirming oesophagitis on histopatholoy.
Oesophagitis is treated by taking a medication that lowers the acid. The most effective medication is a proton-pump inhibitor, which include pantoprazole (Somac®) rabeprazole (Pariet®) ompeprazole (Losec®) or esomeprazole (Nexium®). Peristent oesophagitis can lead to dysplasia, and even cancer, which can be excluded on biopsy.
What is gastritis?
Gastritis may result from imbalance between acid and mucous secretion, but can also result from infection with the bacterial organism Helicobacter pylori. During gastroscopy the appearance of the mucosa lining your stomach can be inspected for any evidence of gastritis, that typically results in red patches (erythema) and occasionally ulceration. Biopsies can be taken, which are painless, and sent for histopathology analysis to determine if there is active gastritis, and if it is associated with Helicobacter pylori infection. If Helicobacter pylori is identified, then eradication therapy will be required. In patients without penicillin allergy by a one to two week course of KlacidHP7® (amoxicillin 1g, clarithromycin 500mg & pantoprazole 20mg) taken twice daily.
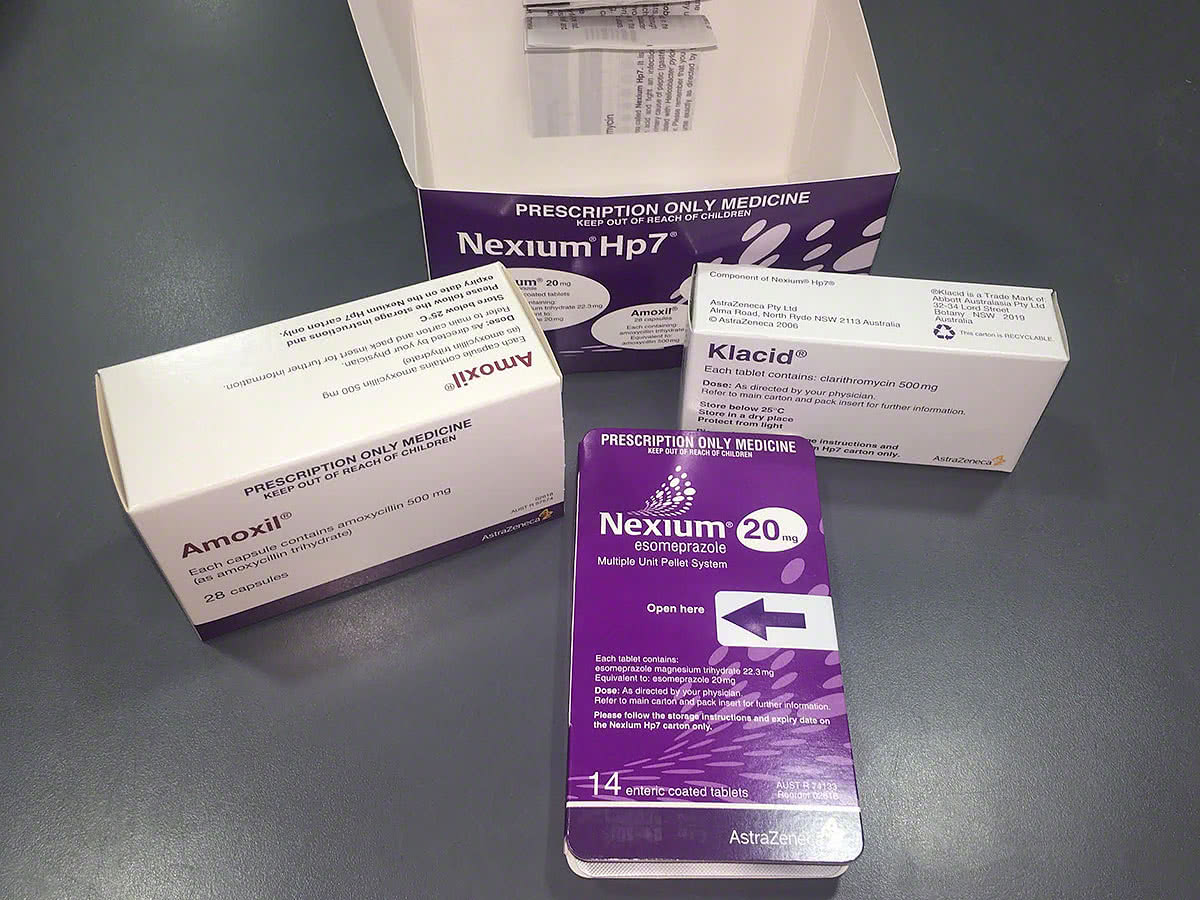
Patients with penicillin allergy can replace the amoxicillin with flagyl 400mg twice daily. Persistent gastritis or helicobactor infection can lead to a chronic gastric ulcer, or even cancer, and these can be excluded on biopsy during your gastroscopy. Confirmation of Helicobactor eradication is done at 6 weeks with an acid breath test, or at 3-6 months with a blood test. These can both be organised by your GP.
What is coeliac disease?
Coeliac disease is an auto-immune disorder of the small intestine that occurs in genetically predisposed people of all ages, from infancy onwards. It results in antibodies against gliadin (a gluten) found in wheat. This leads to sloughing of the mucosal villi of the small intestine. Diarrhoea and bloating can often be the only symptoms. The diagnosis can be made at gastroscopy by taking a biopsy of the small intestine while the patient is under sedation. It is a painless procedure. Once the diagnosis is confirmed, a gluten-free diet can eliminate symptoms.
What is lactose intolerance?
Lactose intolerance is the inability to digest lactose, a sugar found in milk. It is due to a deficiency of the enzyme lactase. It is very common in adulthood, either due to a genetic deficiency in the production of lactase (primary lactase deficiency) or can be a transient condition that results after a recent episode of gastroenteritis. Lactose intolerance can result in abdominal bloating, pain and diarrhoea 30 minutes to 2 hours after consuming dairy products. An intestinal biopsy can confirm lactase deficiency.
Lactase levels vary from one patient to the next, and vary over time, therefore lactose intolerance is not usually an absolute condition. Since lactose intolerance poses no further threat to a person’s health, the condition is managed simply by minimising the symptoms. Therefore, management involves the avoidance of dairy products, substituting them for plant-based milks (e.g. soy milk, rice milk, or oat milk).
What is intestinal metaplasia (IM) of the stomach?
Intestinal metaplasia (IM) of the stomach is a risk factor in developing intestinal-type gastric cancer. It occurs as a result of reduced acidity within the stomach, with gastric mucosa changing its appearance more in keeping with intestinal mucosa. IM is much more common in those with Helicobacter pylori infection, and smokers and alcohol drinkers, and those deficient in essential vitamins including vitamin C found in fresh fruit and vegetables [1]. Bile reflux is also a risk factor for IM. When Helicobacter pylori is present, this needs to be treated with eradication therapy with good evidence that this causes regression of IM [2]. Patients should be encouraged to quit smoking, reduce alcohol intake and there is some evidence that antioxidants (fresh fruit and vegetables and vitamin C) can be protective and reverse IM. Ongoing with Intestinal Metaplasia Surveillance with biopsies of any suspicious plaques is indicated every 3 years, and more often if dysplasia is present.
What should I do before my gastroscopy?
Gastroscopy is performed as a day procedure. Unless you are also having a colonoscopy, no bowel preparation is required prior to your gastroscopy. You must be fasted for 6 hours (no oral food or liquids) prior to your gastroscopy.
What happens during my gastroscopy?
Gastroscopy is quick, easy and safe. You will be sedated during the procedure. You may be asked to bite on a mouth guard prior to the insertion of the gastroscope. If biopsies are taken, they will be painless.
What happens after my gastroscopy?
You will need 1-2 hours to recover after your gastroscopy before being allowed to leave the hospital. You will need someone to pick you up from hospital following your procedure, as it is unsafe for you to travel alone or drive a vehicle. Results of your biopsy should be available within 1 week of your procedure.
References
- You WC, Zhang L, Gail MH, et al. Gastric dysplasia and gastric cancer: Helicobacter pylori, serum vitamin C, and other risk factors. J Natl Cancer Inst 2000;92:1607–12. [PubMed].
- Sung JJ, Lin SR, Ching JY, et al Atrophy and intestinal metaplasia one year after cure of H. pylori infection: a prospective, randomized study. Gastroenterology 2000;119:7–14.
