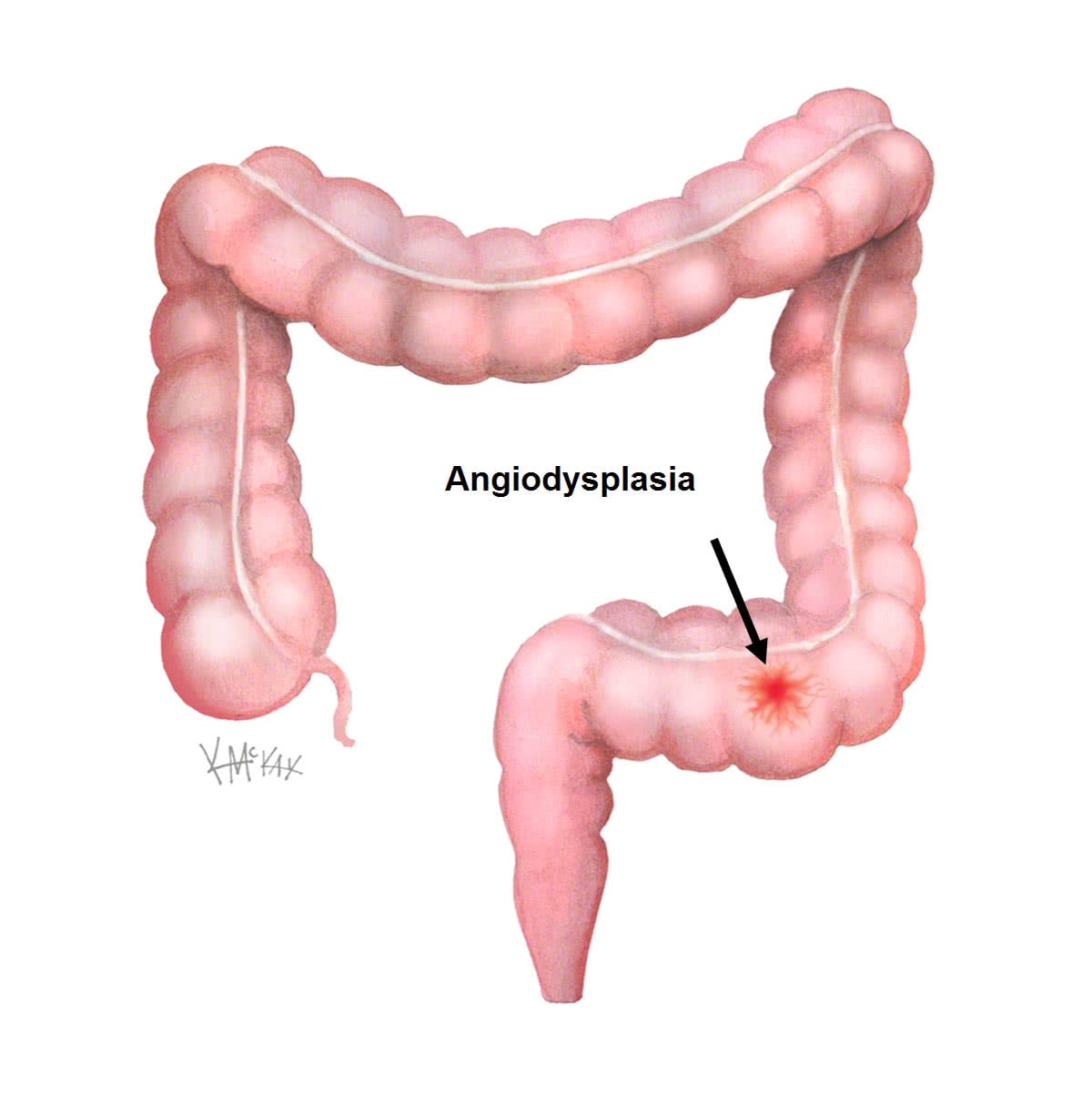
Angiodysplasia is a small vascular malformation of the lining of the colon or rectum. It is a common cause of otherwise unexplained gastrointestinal bleeding and anaemia. Lesions are often multiple, and frequently involve the caecum or ascending colon.
Treatment
Treatment may be with endoscopic interventions or occasionally surgery.
Signs and symptoms
The blood loss can be subtle, with the anaemia the only clinical sign. Faecal occult blood testing (FOBT) is positive when bleeding is active. If bleeding is intermittent the test may be negative at times.
Diagnosis
Although the lesions are typically difficult to find, the diagnosis is usually made at colonoscopy.
Angiography
In cases where a definitive angiodysplastic lesion cannot be seen on colonoscopy, angiography may be necessary. Selective angiography of the mesenteric arteries allows not only for diagnosis of the bleeding angiodysplasia, but also for interventions at time of the procedure.
Pathophysiology
Angiodysplasia is due to abnormal stretching of the vessels in the wall of the bowel, resulting in dilated large vessels (telangiectasia) that are prone to bleeding. They are more common with advancing age, and in those who suffer from constipation.
Treatment
Bleeding may result in anaemia, and If the anaemia is severe, iron replacement and/or blood transfusion may be required.
Colonoscopic ablation with argon plasma coagulation (APC) can be performed with relative ease as a day stay procedure. In severe life threatening cases, resection of the affected part of the bowel may be needed. However, the lesions may be widespread, making such treatment impractical.
Embolisation through angiography is sometimes needed with severely bleeding lesions that cannot be seen on colonoscopy.
