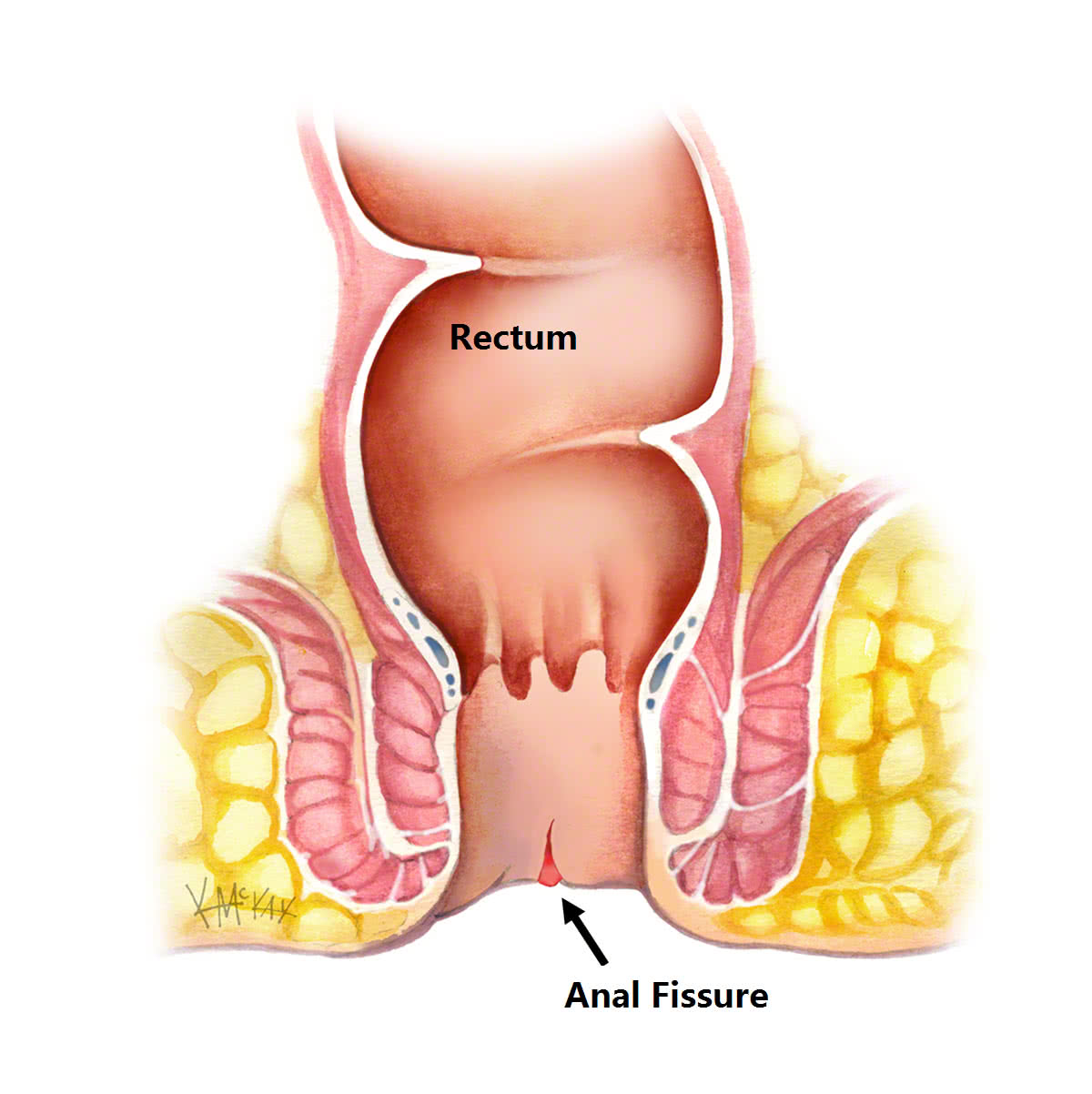
An anal fissure is a tear or split in the lining of the anus (anal mucosa). This if often due to constipation with firm stools tearing the mucosa on defecation. Anal fissures result in severe pain on defecation, with anal sphincter spasm, and further tearing. This often leads to the avoidance of defecation, establishing a vicious cycle of constipation and repeated anal fissuring.
Symptoms
Symptoms include pain and bleeding from the anus when passing a bowel motion.
Cause
Common causes in adults include constipation and trauma to the anus. Rarely it is due to Crohn’s Disease of the anus. Around half of cases heal by themselves with proper self-care and avoidance of constipation. However, healing can be a problem if the pressure of passing bowel motions constantly reopens the fissure. Treatment options include the use of bulking agents such as Metamucil ® or Fibogel® to loosen the stool and laxatives such as lactulose (Duphulac®) or osmotic laxatives such as Movicol®. The topical application of medications to relax the sphincter such as Rectogesic® or diltiazem may help. These can also be combined with botulin toxin (Botox®) injections to the internal sphincter to allow temporary relaxation of the anus to allow for healing of the fissure. If these measures failure, surgery may be indicated, where a small proportion of the internal sphincter is cut.
Complications
Acute anal fissures are usually a benign condition not associated with more serious diseases, such as bowel cancer. Failure to heal can result in the development of a chronic anal fissure. Over time, this can cause extensive scar tissue at the site of the fissure (sentinel pile). Rarely, anal fissures can form an anal fistula (an abnormal tract that joins the internal anus to the external skin surrounding the anus).
Diagnosis
An anal fissure is largely a clinical diagnosis based on the typical history including pain and bleeding on defecation, along with the classic features of pain on examination, and a visible fissure in the midline of the anus. Commonly, examination is poorly tolerated and proper diagnosis requires examination under anaesthetic.
Treatment
Lifestyle modification
Simple lifestyle modifications to prevent constipation include drinking plenty of water (six to eight glasses of water a day), having a diet high in fibre, and exercising regularly. To allow the fissure to heal we suggest showering or bathing, or using baby wipes after every bowel motion and taking regular warm-to-hot salt water (Sitz) baths, which involves sitting in a shallow bath of water for around 20 minutes. This is soothing as well as cleansing.
Medical management
Once a fissure is established, the above measures rarely result in healing, and medical treatment is often required. Stool softeners containing non-soluble fibre including natural psyllium husk (Metamucil®) or ispaghula husk (Fibogel®) are recommended. Laxatives are commonly required and include lactulose (Duphalac®) sterculia (Normacol®) or osmotic agents containing magroglol polymers and sodium phosphate (Movicol®). Pain relief may be required and include over the counter non-opioid based analgesics including non-steroidal medications such as ibuprofen (Brufen®) and simple paracetamol (Panadol®). Opioid medications containing morphine-like agents should be avoided as they cause constipation, which exacerbates the condition.
Topical gels
Topical nitrates such as 0.2% glycerine trinitrate (Rectogesic®) and 1% isosorbide dinitrate (Isordil®) work by relaxing the internal sphincter, and preventing spasm. Headaches are a side effect of Rectogesic® and are less common with Isordil®. In breast-feeding mothers, nitrates should not be used, and calcium channel blockers (diltiazem) in 2% gel form is an effective alternative. These ointments are all applied to the anal sphincter three times a day, and must be used for 6 weeks for success. These agents are effective in over half of cases [1].
Neurotoxin injections
Neurotoxin (Botulin toxin A) injections work by temporarily paralysing a portion of the internal sphincter muscle. Botox has the advantage of being effective in 60-80% of cases as well as being reversible and repeatable. Unfortunately, it is not covered by private health insurance or medicare in most hospitals, and costs $500 per injection. There have been reports of temporary incontinence in 20% of patients [1]. Combination Botulin toxin A injections and topical gels such as those already mentioned are more likely to work than either on its own.
Surgery
Surgery is indicated for the anal fissure that fails to heal despite those non-operative measures described above. The chronic anal fissure present for more than 6 weeks, or the painless fissure that is not in the midline may require a biopsy to exclude Crohn’s disease or squamous cell carcinoma.
Lateral sphincterotomy
Relaxation of the anal sphincter may be achieved by performing a lateral sphincterotomy. In this procedure less than a third of the inner anal sphincter is divided at the level of the anal fissure, to provide relief from anal sphincter spasm to allow healing of the fissure. This procedure is called a lateral sphincterotomy and is extremely effective with a success of over 90%. The long-term side effects include incontinence in up to 3% of cases.
Anoderm or rectal advancement flaps
Anal fissures that fail to heal with the above measures, may need to be surgically removed, and repaired using a flap. This procedure is particularly suited for the chronic painless fissure, where anal pressures are normal suggesting that anal spasm is not the cause. In this procedure, the fissure and associated scar tissue is removed, and the lining (mucosa) of the anus or rectum along with the underlying muscle is mobilised as a flap to cover the defect.
What to expect pre and post operatively for anal fissure surgery
Fasting and Bowel Preparation
Unless you are also having a colonoscopy, a normal diet without a bowel prep, is required the day before surgery. You need to fast from midnight the night before if your surgery is scheduled for the morning, or from 7am if scheduled for the afternoon. You will be admitted as a day-stay procedure. You will receive a fleet® enema 1 hour prior to your operation.
Recovery and transport
Following your procedure, you will recover for an hour until the effects of sedatives have worn off. You should not drive yourself home after your procedure and should have someone organised (a friend or relative) to accompany you.
Bleeding
Spotting of blood will occur for 5 days following your procedure, and a sanitary napkin will be needed to prevent staining of your underwear. Bleeding will typically occur after opening your bowels. If the bleeding is more than a couple of teaspoons a day, notify your surgeon.
Laxatives
You should remain on regular laxatives and simple analgesics for 1 week. A tablespoon of natural psyllium husk (Metamucil® or Fibogel®) twice daily, and 30ml of lactulose (Duphalac®) twice daily is recommended.
Pain control
For pain, continue regular topical application of glycerine trinitrate Rectogesic®) three times daily for up to six weeks following your surgery is recommended. Simple oral analgesics may occasionally be needed, and a non-steroidal is recommended such as 400mg of ibuprofen (Brufen®) along with 2 tablets of paracetamol. This should be only if required, and can be taken up to three times a day for five days. Opioid medications (Endone) are rarely indicated and should be avoided as they cause constipation.
Sitz Baths
Twice daily warm to hot salt-water (Sitz) bathing to the anal region is soothing and antiseptic, and should be done for 1 week following your procedure. Put a handful of salt into a shallow bath of warm-to-hot water and sit there for 10-15 minutes.
Follow-up
You should follow up with your colorectal surgeon in 6-8 weeks following your surgery to review your wound and discuss further management if indicated.
References
-
Perry WB. Dykes SL. Buie WD. Rafferty JF. Standards Practice Task Force of the American Society of Colon and Rectal Surgeons. Practice parameters for the management of anal fissures (3rd revision). Diseases of the Colon & Rectum. 53(8):1110-5, 2010 Aug.
