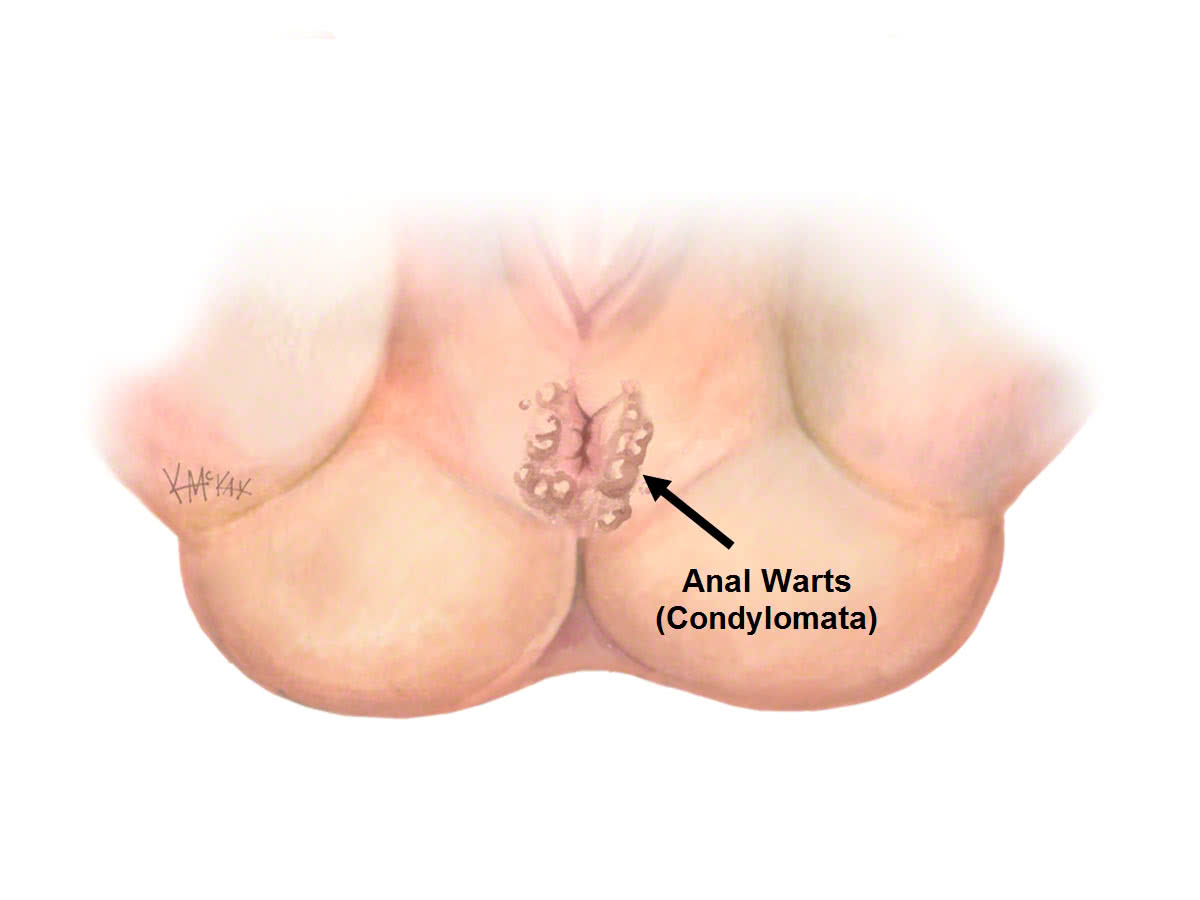
Anal warts (also called Condyloma Acuminata) result from previous infection with the Human Papilloma Virus (HPV).
Cause
Over 90% of anal warts are due to infection with HPV subtypes 6 & 11. These are rarely associated with anal cancer. Less than 10% of anal warts are due to infection with HPV Serotypes 16 & 18. However, serotypes 16 & 18 are both strongly associated with risk of developing anal cancer. Immunosuppressed patients (e.g. HIV) are at higher risk of infection. The highest risk population are the HIV male population, particularly those men who have sex with men (HIV – MSM).
Symptoms
Perianal warts frequently itch, bleed and result in perianal wetness. There may be an associated lump. They are often confused for a haemorrhoid.
Investigation
Biopsy and Histopathology
Peri-anal warts are usually clinically apparent. They range from small pinkish-white small lesions to much larger lesions that are cauliflower in appearance. Their diagnosis is confirmed on histology from biopsy.
Viral Testing
Viral tests for HPV virus are available which are able to differentiate the serotype of HPV responsible. However, currently, there is no consensus opinion or convincing evidence of a benefit of routine testing for viral HPV serotypes. This is because viral serotypes are often cleared over time, and with ongoing sexual activity and new exposures, infection with different serotypes or a variety of serotypes may occur.
PAP smear
Although the PAP smear is currently used in Australia for cervical cancer screening, its role for anal cancer is less clear. PAP smear testing mainly has a role as a research tool in screening for Anal Intraepithelial Neoplasia (AIN). The poor sensitivity of the PAP smear remains an issue.
High Resolution Anoscopy
High resolution anoscopy with acetic acid staining is for excluding Anal Intra-epithelial Neoplasia (AIN) in high risk individuals such as HIV positive men who have sex with men (HIV-MSM). There are currently only five high resolution anoscopes in Australia, limiting their use, and currently there are no Australian guidelines on how often this should be performed.
Course
Most non-immunocompromised patients clear their warts over time, although repeated treatments may be needed to obtain full clearance. There is a long-term risk of Anal Intra-epithelial Neoplasia (AIN) with warts, particularly those due to HPV serotypes 16 & 18. High Grade Anal Intraepithelial Neoplasia (AIN) has a 10% chance progressing to Anal Cancer over a 5-year period.
Prevention
Anal warts are sexually transmitted, and spread by direct skin contact and are avoided by having protected intercourse. Barrier methods (condoms) help prevent against, but do not eliminate the risk of wart virus transmission.
Vaccination
The HPV vaccine (Gardasil®) prevents infection against HPV serotypes 6, 11, 16 & 18 known to cause warts. But more importantly the HPV vaccine protects against serotypes 16 & 18 which are known to cause anal cancer. To be most effective, vaccination should be given early in life, preferably prior to sexual activity before exposure to the wart virus. There is still some benefit of vaccination to those who already have anal warts or high grade dysplasia, as the vaccine may allow clearance of the virus, and also protect against other serotypes they may not have come into contact with.
Since February 2013, free HPV vaccine (Gardasil®) has been provided through the school-based program for all males and females aged 12-13 years occurring in the first year of secondary school. The Gardisil® vaccine costs $153.43 each, and is recommended repeating at 3 and 6 months.
Medical management
Medical therapy with topical agents such as podophyllin resins (Wartkill®), with or without acetic acid, tend to fail, and there are concerns about systemic toxicity when applied to large areas. It is therefore only suitable for small lesions, and should be applied once a week, with numerous treatments usually required.
Podophyllotoxin is more effective being the purified anti-wart compound, and is available in 0.5% solution (Condyline® paint). This can be administered twice a day for 3 days, followed by 4 days of no treatment, and this cycle is repeated for four cycles. It is successful in less than 70% of cases and causes ulceration in 10-20% of cases.
Surgical management
Surgical management mainly consists of electro-cautery (diathermy) to de-bulk or reduce the size of the lesions, or excision, where the entire lesions is removed, including a full thickness excision of involved skin. Whilst diathermy to debulk the size of warts is less painful than excision, it is also unlikely to be curative. Excision of the entire wart with full-thickness excision of skin, is quite painful, and 5 days of analgesics, rest, and salt water baths is required. It is not uncommon for small warts to return, and these require excision as soon as they are noticed, to allow complete eradication of the wart virus.
What to expect pre and post operatively for anal wart surgery
Fasting and Bowel Preparation
Unless you are also having a colonoscopy, a normal diet without bowel preparation, is required the day before surgery. You need to fast from midnight the night before if your surgery is scheduled for the morning, or from 7am if scheduled for the afternoon. You will be admitted as a day-stay procedure. You will receive a fleet® enema 1 hour prior to your operation.
Recovery and transport
Following your procedure, you will recover for an hour until the effects of sedatives have worn off. You should not drive yourself home after your procedure and should have someone organised (a friend or relative) to accompany you.
Bleeding
Spotting of blood will occur for 5 days following you procedure, and a sanitary napkin will be needed to prevent staining of your underwear. Bleeding will typically occur after opening your bowels. If the bleeding is more than a couple of teaspoons a day, notify your surgeon.
Laxatives
You should remain on regular laxatives and simple analgesics for 1 week. A tablespoon of natural Isphagula husk (Metamucil® or Fibogel®) twice daily is usually enough. If constipation develops, 30ml of lactulose (Duphalac®) twice daily is recommended.
Pain control
The amount of pain will depend on the amount of surgery performed to the perianal region. If only small excisions are performed, there may be very little pain, but for large ulcers to the anal region pain may be an issue. For pain, a non-steroidal is recommended such as 400mg of ibuprofen (Brufen®) along with 2 tablets of paracetamol. This should be taken regularly three times a day for five days. Opioid medications (Endone®) may sometimes be needed, but should be used sparingly as they cause constipation.
Sitz Baths
Twice daily warm to hot salt water (Sitz) bathing to the anal region is soothing and antiseptic, and should be done for 1 week following your procedure. Put a handful of salt into a shallow bath of warm-to-hot water and sit there for 10-15 minutes.
Follow-up
You should follow up with your colorectal surgeon in 6-8 weeks following your surgery to review your wound and discuss further management if indicated.
