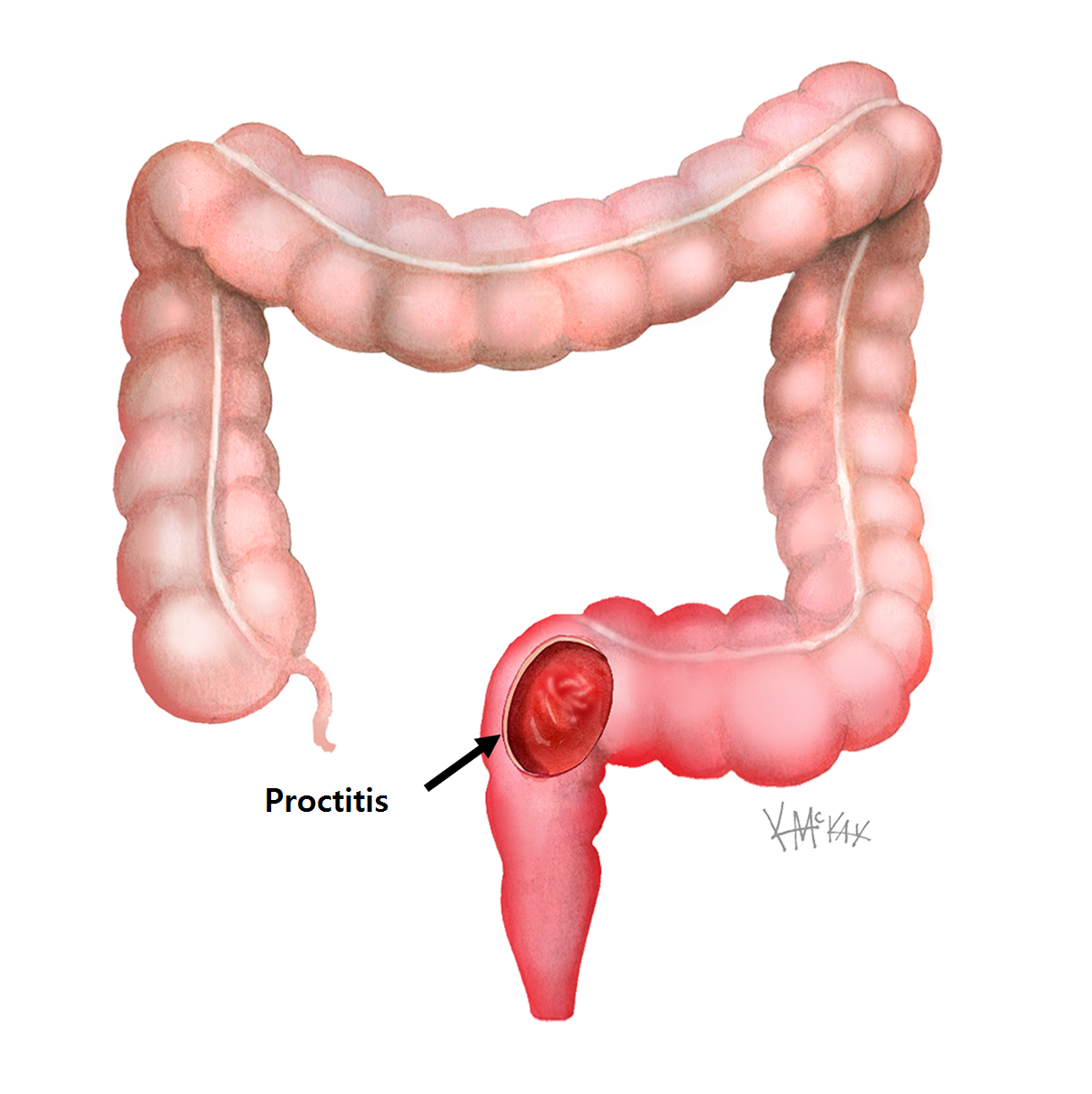
Proctitis is inflammation of the lining (mucosa) of the rectum.
Cause
There are many causes of proctitis, however in some cases the exact cause is still not known. Inflammatory bowel disease (IBD) is responsible for the vast majority of cases of proctitis, however the exact cause of IBD remains elusive. Ulcerative colitis and Crohn’s disease are two common forms of IBD responsible for proctitis. A third form of IBD is “indeterminate colitis” where the criteria to diagnose as either ulcerative colitis or Crohn’s disease are not met. Ulcerative colitis always causes proctitis, whereas Crohn’s disease can involve any part of the gastrointestinal tract (GIT) and doesn’t always cause proctitis. Others less common causes of proctitis, include those due to an injurious agent such as infection, radiation, and trauma.
Radiation proctitis
Radiation proctitis is most commonly a complication of radiotherapy received for prostate cancer (in men) and cervical cancer (in women). With increased use of radiotherapy, its incidence is on the rise.
Infective proctitis
Infective causes of proctitis include those same infections that cause infectious gastro and include viruses such as rotavirus, and bacteria such as clostridium difficile, shigella, campylobactor, and amoebae such as yersinea and entamoeba histolytica. Other infectious causes of proctitis include those due to sexually transmitted diseases (STDs), such as gonorrhoea, chlamydia, and herpes simplex virus 1 and 2.
Effects of proctitis
Proctitis causes a red and “angry” rectum, much like a rash or a sunburn of the lining (mucosa) of the rectum that is friable and easily bleeds and ulcerates. In Ulcerative colitis the rectum is always involved resulting in proctitis, and any colonic involvement is continuous with the rectum, whereas in proctitis due to Crohn’s disease, there may be patches of uninvolved mucosa between involved mucosa, (so called “skip lesions”). In ulcerative colitis, the proctitis is not as deep, involving only the superficial mucosa and submucosa. In Crohn’s disease the whole thickness of the rectal wall is involved. Crohn’s proctitis therefore is more likely to result in deep ulcers, that often are linear (serpigenous).
Proctitis due to irradiation has many similar features to that due to IBD. A history of previous exposure to radiotherapy and the onset of proctitis following this, along with the absence of typical IBD features on biopsy all favour a diagnosis of radiation proctitis.
Presentation
Bloody mucous discharge is the commonest symptom of proctitis. There may also be some associated diarrhoea, that is often blood-stained (dysentery). Fatigue and light-headedness, due to chronic blood loss and anaemia, can also result.
Diagnosis of proctitis
Stool cultures should be sent to test for common infective agents that may be responsible. Colonoscopy is necessary not only to make the diagnosis of proctitis, but also to exclude other conditions that can cause rectal bleeding. Colonoscopy also allows for real time images to be taken of the lining of the rectum which has a characteristic appearance with granular friability, bloody mucous discharge, and contact bleeding when the colonoscope touches the mucosa. Colonoscopy also allows for biopsies to be taken to allow definitive examination under a microscope, and to send the tissues for culture to exclude infective causes.
Is there a risk of cancer with proctitis?
Longstanding proctitis, particularly those caused by inflammatory bowel disease (IBD) are associated with an increased risk of cancer transformation. The progression from proctitis to cancer is over a period of time. Early precancerous changes (dysplasia) begins as mild before becoming moderate, and in some cases becomes severe dysplasia, before finally becoming invasive cancer. Colonoscopy allows for visual inspection of the colon and rectum, as well as allowing for biopsies to be taken, to make sure that high grade dysplasia or cancer are not present.
Management of proctitis
Infective proctitis need to be identified, and the infective agent treated with antibiotics, although these represent the minority. Most other non-infectious cases of proctitis settle with suppositories or rectal foam containing prednisone (Predsol®). In cases due to inflammatory bowel disease (IBD) enemas containing salazopyrine(Salofalk®) may be used.
Irradiation proctitis frequently resolves in the months following radiation treatment. Cases which persist can be difficult to treat. Troublesome bleeding can improve with topical application of formalin, or with APC (argon-plasma coagulation) or laser.
Role of surgery for proctitis
Occasionally surgery is indicated for severe cases of proctitis due to inflammatory bowel disease (IBD). In other cases surgery is indicated to reduce the risk of cancer where high grade dysplasia is found on routine biopsies.
In ulcerative colitis the rectum can be removed completely and a new rectum constructed using small bowel (called a “J pouch”) which is then joined directly to the anus. There is some evidence that this can also be done for “indeterminate proctitis”, however formation of a “J-pouch” is associated with a high failure rate when used for proctitis due to Crohn’s disease, and is generally discouraged.
